Sepsis, the body’s life-threatening response to infection affecting about 1.7 million adults in the United States each year, can lead to multisystem organ failure with a high mortality rate.
No targeted therapeutics against this condition have been developed in the last decades. Now, however, a team led by biomedical scientists at the University of California, Riverside, offers some hope for future treatment during sepsis awareness month.
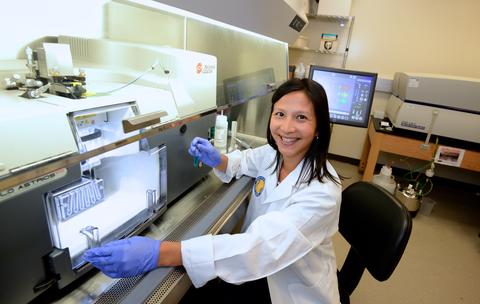
The researchers, led by Meera Nair and Adam Godzik in the School of Medicine, identified molecular biomarkers, pathways and immune cell dynamics associated with sepsis that could be therapeutically targeted to prevent the condition from leading to death. These blood cell biomarkers — the protein CD52 in lymphocytes; and the protein S100A9 involved in inflammatory processes — are present in all blood cells but highly expressed in people with sepsis. How these biomarkers change early in sepsis — specifically, within the first six hours — could determine whether the patient survives or dies.
“These biomarkers were found to uniquely change within six hours in the blood of patients with sepsis and affected specific cellular pathways in specific immune cells,” said Nair, an associate professor of biomedical sciences, who co-led the study published in the Journal of Leukocyte Biology. “Changes in CD52 expression were associated with good outcomes, which means promoting the activation of protective immune cells. S100A9, on the other hand, acted as a molecular driver of fatal sepsis. We appear to have found a molecular driver and a molecular protector of sepsis.”
According to Nair, the team also found the molecular pathways for fatal sepsis and COVID-19 converge.
“Severe COVID appears to trigger molecular pathways identical to sepsis,” she said. “Further analysis of these pathways can help us diagnose and treat both diseases.”
In particular, the research team also found that in people with sepsis, blood platelets — cell types involved in normal blood flow and coagulation — lost their function, as they do in COVID patients. The researchers argue that if the platelets’ function could be restored by targeting the main regulators of this process, it could promote survival in both sepsis and COVID.
Nair explained that when a patient is diagnosed with sepsis and admitted to the intensive care unit, physicians use clinical scoring systems, such as the APACHE-2 and SOFA scores, to help predict severity of illness and probability of mortality.
“Clinicians still cannot predict whether the patient is going to survive or die and what specific treatment to give that may improve their survival chances,” she said. “There is no way, unfortunately, of triaging the patients to figure out if they would benefit from one treatment versus another. We wanted to address this by finding molecular biomarkers that are better predictors of whether a patient survives or dies. We appear to have found some candidates.”
The study, done in partnership with clinicians at the Riverside University Health System, or RUHS, involved sampling the blood of five patients with sepsis. Dr. Walter Klein, the paper’s co-author and a pulmonologist at RUHS, noted clinical scoring systems do not provide specific therapeutic targets for patients.
“From a clinical perspective, the treatment of sepsis largely focuses on early recognition, early systemic antibiotics/source control of the infection, and support of failing organ systems,” he said. “What is missing in the clinical arena are specific therapies that reverse the patient’s dysregulated immune response to infection. The importance of basic science research like this is to hopefully find individualized treatments one day where we can rapidly reverse the patient’s multi-organ failure and prevent mortality.”
Unlike other studies that analyzed blood samples from patients with sepsis at time zero, when patients are first diagnosed with the disease, the research team analyzed blood samples of sepsis patients at time zero and six hours later — two different time points from differing outcomes in sepsis.
“We have snapshots in two time-steps that show us how the biomarkers are evolving,” said Godzik, the Bruce D. and Nancy B. Varner Presidential Endowed Chair in Cancer Research at UCR and a professor of biomedical sciences, who co-led the study. “We can enhance this evolution in the right direction, toward survival. If the patient is heading in the wrong direction, toward fatality, we can intervene to change the trajectory of the disease. With this work, we have gone beyond the static snapshot and moved into a more dynamic process.”
Blood samples obtained from RUHS were processed at a single-cell sequencer at UCR, allowing the researchers to understand the behavior of each cell rather than an average of all cells.
“We found that many cell types behaved differently in sepsis,” said Xinru Qiu, the co-first author of the paper and a graduate student in Godzik’s lab. “Using single cell sequencing, we could separately track the trajectory of different cell types. Single-cell resolution is like having a street-level view of an area versus a satellite view of it, and an understanding of what each cell contributes were key in helping us find our results.”
According to Godzik, when news reports note someone has died of complications from an infection, it generally means the person died of sepsis.
“Thirty percent of all deaths in hospitals are caused by sepsis,” he said. “Sepsis is an unmet need with no treatment. Our work offers a path to treatment because we have extended the view from single molecules to processes in cells. After all, it is the molecular pathways involved that can be interrupted. Oftentimes, people think if a gene is a biomarker of a disease, a drug should target it. Well, not necessarily. If the bumper of your car — the tag or marker — is destroyed in a car accident, you may have need to fix the brakes — the pathway.”
Nair stressed that the study was possible only through a multidisciplinary approach.
“As an immunologist, I teamed up with Adam, who is a computational biologist, and with RUHS clinicians,” she said. “It’s only through such collaborative work that we can start to unravel the complexity of fatal sepsis, offering insight into new treatments that could change the trajectory of sepsis patients who may face a fatal outcome.”
Next, the researchers plan to focus on similarities between sepsis and COVID-19 and have already begun research funded by the Center for Health Disparities Research at UCR.
“We are doing a molecular analysis of the long-term effects of COVID-19 on immune homeostasis,” Nair said. “We would like to see if our sepsis research findings could apply also to COVID-19.”
Nair, Godzik, Qiu, and Klein were joined in the research by Jiang Li, the co-first author of the research paper, and Lukasz Jaroszewski at UCR; and Drs. Jeff Bonenfant and Aarti Mittal at RUHS.
The research was supported by the UCR School of Medicine, a School of Medicine Dean’s innovation grant to Bonenfant, and the National Institutes of Health. Bonenfant completed his medical residency at the UCR School of Medicine in 2018.
The research paper is titled “Dynamic changes in human single cell transcriptional signatures during fatal sepsis.”
Header image by Sharon McCutcheon on Unsplash