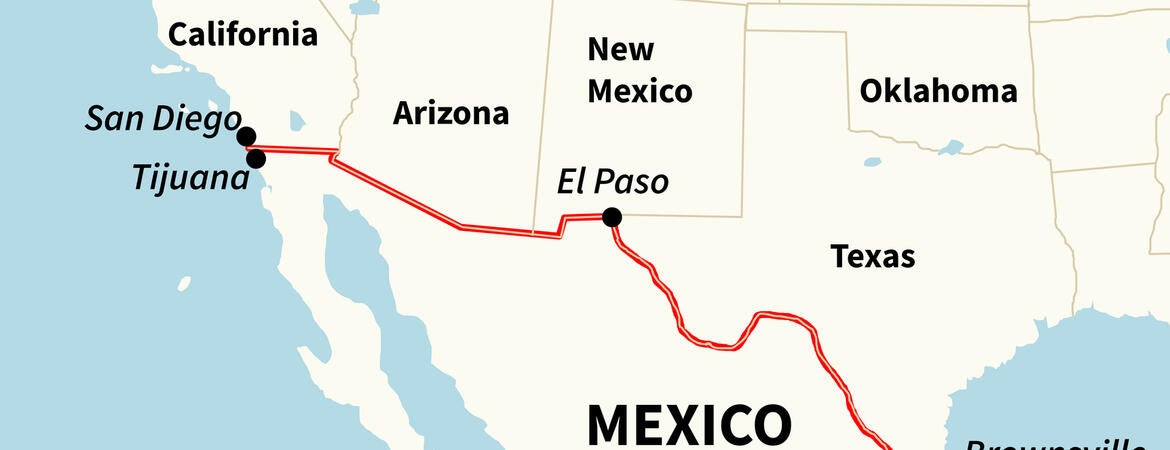
In unincorporated communities in the United States-Mexico borderlands, historically and socially marginalized populations become invisible to the healthcare system, showing that geography acts as a structural determinant of health for low-income populations. So concludes a study by a University of California, Riverside, team that focused its attention on the borderland in Southern California, specifically, eastern Coachella Valley.
From September to December 2020, the team, led by Ann Cheney, an associate professor of social medicine, population, and public health in the School of Medicine, conducted interviews in collaboration with María Pozar, a community investigator and CEO of Conchita Servicios de la Comunidad, with 36 Latinx and Indigenous Mexican caregivers of children with asthma or respiratory distress. The researchers found communities in the “colonias” (unincorporated areas in the borderlands) lack basic critical infrastructure including healthcare access.
The U.S.-Mexico borderland is home to nearly 2.7 million Hispanic or Latinx individuals. The immigrant population in the colonias has limited English proficiency, health literacy levels, and income, and lower levels of formal education. Many are undocumented.
“Our work shows the importance of geography in health and how geography acts as a structural determinant of health,” Cheney said. “For example, foreign-born caregivers who speak Spanish or Purépecha prefer to take their children across the U.S.-Mexico border for respiratory health care because physicians there provide them with a diagnosis and treatment plan that they perceive improves their children’s health.”
The study, published in the journal Social Science & Medicine, found the caregivers perceive U.S.-based physicians as not providing them with sufficient information since most physicians do not speak their language and do not adequately listen to or are dismissive of their concerns about their children’s respiratory health. The caregivers perceive Mexican-based physicians as providing them with a diagnosis and treatment plan, whereas U.S.-based physicians often prescribe medications and provide no concrete diagnosis.
“Further, only those with legal documentation status can cross the border, which contributes to disparities in children’s respiratory health,” Cheney said. “Thus, caregivers without legal status in the U.S. must access healthcare services in the U.S. for their children and receive, what these caregivers perceive, as suboptimal care.”
Cheney added she was surprised to learn that caregivers who did not have legal documentation status in the U.S. asked trusted family and friends to take their children across the border to receive healthcare services for childhood asthma and related conditions.
“Geography, meaning living in unincorporated communities, harms health,” she said. “Geography and the politics of place determines who can and cannot cross borders.”
Study participants discussed the distance they needed to travel to pediatric specialty care for the care and management of their children’s respiratory health problems. Some commented on the lack of interaction and communication with physicians during medical visits. Some participants commented on the lack of physicians’ knowledge about the connections between their children’s exposure to environmental hazards and poor respiratory health and allergic symptoms.
The research took place in four unincorporated rural communities — Mecca, Oasis, Thermal, and North Shore — in eastern Coachella Valley, along the northern section of the Salton Sea. People living in the colonias here are subject to the health effects of environmental hazards. Many are farmworkers living and working in the nearby agricultural fields. Most of the workforce lives in mobile parks and below the federal poverty line.
“In addition to toxic water and dust from the Salton Sea, other environmental health hazards, such as agriculture pesticide exposure, waste processing facilities, and unauthorized waste dumps, also contribute to this community’s high incidence of poor respiratory health,” said Gabriela Ortiz, the first author of the research paper and a graduate student in anthropology who works with Cheney. “These communities are vulnerable to the policies and governing decisions around exposure to environmental hazards and infrastructure development. The absence of infrastructure and lack of healthcare infrastructure limits their access to primary care and specialty care services.”
Ortiz explained that anthropologists and social scientists have long argued that environmental injustices are a product of structural violence.
“This is indirect violence caused by social structures and institutions that prevent individuals from meeting their basic needs because of political economic domination and class-based exploitation,” she said. “Understanding the complex interplay between geography, borderlands, and health is essential for coming up with effective public health policy and interventions.”
The title of the research paper is “Seeking care across the US-Mexico border: The experiences of Latinx and Indigenous Mexican caregivers of children with asthma or respiratory distress.”
Cheney, Ortiz, and Pozar were joined in the study by Ashley Moran and Sophia Rodriguez of UCR.
The study was funded by the National Institutes of Health/National Institute of Minority Health and Health Disparities.
Header image credit: Arseniy45/iStock/Getty Images Plus.