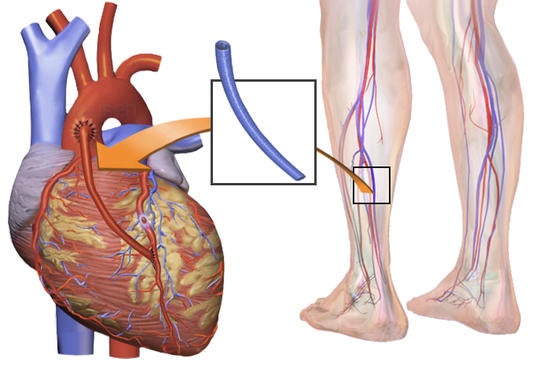
Women have conventionally been considered a risk factor for coronary artery bypass grafting (CABG), a type of open-heart surgery that improves blood flow to the heart. But a research paper by an international team of researchers, including two cardiologists at the University of California, Riverside, argues that sex should not influence treatment decisions about CABG.
Investigating the association of sex and the long-term benefit of CABG in male and female patients with ischemic left ventricular dysfunction enrolled in the STICH trial (Surgical Treatment for Ischemic Heart Failure Study), the largest surgical trial testing medical therapy versus CABG in ischemic diseases affecting the heart muscles, the researchers found that sex is not associated with the effect of CABG on mortality due to all causes, cardiovascular mortality, cardiovascular hospitalization, or surgical deaths in patients with ischemic left ventricular dysfunction.
“Despite worse risk factors, women fared better than men in our study,” said Dr. Ramdas G. Pai, a professor of cardiology at the UCR School of Medicine and a coauthor on the study published in Circulation and led by Dr. Ileana L. Piña of the Albert Einstein College of Medicine in New York. “The surgical complications were similar in both men and women. This refutes the prevailing myth that women do worse than men when they need CABG and must, therefore, be denied surgery.”
The study involved 1,212 patients with ischemic left ventricular dysfunction, of which 148 were women. Roughly half the men and women were randomly selected and given CABG and medical therapy (MED); the rest were given MED alone. The researchers then compared the long-term (10-year) outcomes with each treatment according to sex.
“We wanted to explore the following questions in these patients: Is surgery beneficial? Should you take just medication? Or should that be supplemented by surgery?” said Pai, who chairs the Division of Clinical Sciences and Department of Internal Medicine. “We found that surgery was a far superior option for both men and women. Despite women having higher risk profile for heart disease than men, women do not have a higher surgical risk. Indeed, after 10 years of follow-up, women had better survival with surgery, with significantly lower rates of long-term all-cause mortality and cardiovascular mortality than men. Therefore, sex should not influence their treatment decisions where CABG is concerned.”
Generally, women are underrepresented in clinical trials. Data based on predominantly male subjects in cardiovascular clinical trials have been extrapolated to women. Coronary heart disease, widely seen as a problem for men, resulted in women being understudied, underdiagnosed, and undertreated.
“We all need to recognize that the female heart is vulnerable to coronary heart disease and that appropriate intervention, such as CABG, has the potential to delay or avert coronary events,” Pai said. “Even when coronary heart disease signs are present, women often do not get medical attention. And when they get medical attention, their physicians may not consider them for surgery. Physicians should consider them to be appropriate surgical candidates.”
Piña and Pai were joined in the study by Dr. Padmini Varadarajan at UCR and researchers at Duke University School of Medicine, Durham, N.C.; National Institute of Cardiology, Warsaw, Poland; Medical University of Vienna, Austria; Instituto Dante Pazzanese de Cardiologia, Sao Paulo, Brazil; Istituti di Ricovero e cura a Carattere Scientifico Policlinico San Donato, Milan, Italy; Medical University of Silesia, Katowice, Poland; University of Trier, Germany; Dedinje Cardiovascular Institute, Belgrade, Serbia; University Hospital Favaloro Foundation, Buenos Aires, Argentina; University of Sao Paulo Medical School, Brazil; National Institutes of Health, Bethesda, Md.
The study was funded by the National Institutes of Health.