Memory Matters
Advancements in research across UCR offer new hope for Alzheimer’s disease and other causes of dementia
By Iqbal Pittalwala | Photos by Stan Lim
I lana Bennett’s interest in studying Alzheimer’s disease is deeply personal. Since she was a young girl, she has been drawn to older adults, valuing their knowledge and cherishing the relationships she has had with them, particularly with her grandparents.
“This connection drives my commitment to understanding and addressing the challenges of Alzheimer’s disease,” said Bennett, an associate professor of psychology in the College of Humanities, Arts, and Social Sciences and co-chair of the UCR Aging Initiative. “It has made me passionate about promoting successful aging and improving the quality of life for older individuals.”
Alzheimer’s disease, or AD, is the most common cause of dementia, a general term for loss of memory and other cognitive abilities that seriously interfere with daily life. AD is a progressive disease where dementia symptoms gradually worsen with time. Accounting for 60-80% of dementia cases, AD has no cure, but treatments are available. It is projected to affect more than 100 million people worldwide by 2050.
Bennett is one of several UCR researchers across multiple colleges and departments working toward better understanding and treating AD and dementia. Her primary motivation for researching the disease stems from its profound impact on memory as we age. AD is often associated with one of our greatest fears — losing our cognitive functions, she said, which makes it a critical area of study.
“It’s common for even minor memory lapses to be attributed to Alzheimer’s, while other factors such as sleep deprivation or medication side effects might be overlooked,” she said. “The prominence of Alzheimer’s in public consciousness and its significant negative effects on life make it a particularly compelling subject for research.”
Bennett’s research focuses on understanding specific learning and memory processes in older adults, with the aim of gaining insights into how these processes are affected in AD. She also studies populations with mild cognitive impairments, which are often early indicators of AD. Her lab examines various aspects of the disease, including inflammation and brain perfusion — blood flow delivering oxygen and nutrients to the brain’s tissues.
“Some of our work involves studying inflammation’s role in Alzheimer’s, a topic that is gaining increasing attention,” she said. “Traditionally, Alzheimer’s research centered on proteins like amyloid and tau, with the amyloid cascade hypothesis suggesting that amyloid accumulation triggers a cascade of detrimental effects, ultimately impairing cognition.”
The field of AD research has evolved significantly and now recognizes that multiple pathologies contribute to the disease. While the amyloid cascade hypothesis was once central, evidence over the past two decades has shown that amyloid alone does not fully explain the clinical symptoms of the disease. Recent research focuses on a combination of markers such as tau accumulation, neurodegeneration, vascular deficits, and inflammation in both the brain and peripheral systems.
One of the most formidable challenges facing public health in the 21st century, Alzheimer’s disease robs people of their individuality, capabilities, and cherished memories. It also burdens families and societies with an emotional and economic toll. An estimated 6.9 million Americans aged 65 and older are living with Alzheimer’s dementia today. This number could grow to 13.8 million in the U.S. by 2060.

In his practice at UCR Health, neuropsychologist Dr. David Franklin frequently encounters patients with AD. A health sciences clinical professor in the Department of Psychiatry and Neuroscience at UCR’s School of Medicine, Franklin began studying AD in the late 1990s at UC Irvine, where he was involved in studies on new medications for treating the disease. His grandparents had Alzheimer’s disease, which boosted his commitment to understanding and researching treatments.
“Alzheimer’s can begin in someone as early as their mid-50s,” he said. “By the age of 90 and above, there is a 50% chance of developing the disease. Early signs include repeated questions, frequent forgetting of appointments, and difficulty recalling recent events or places visited.”
Treatment options for AD include acetylcholinesterase inhibitors, such as Aricept. According to Franklin, these medications help slow disease progression and can improve quality of life for up to a year, but they do not reverse the disease. Newer treatments, including antibodies that are delivered via transfusions, are used in the earlier stages to slow progression, but they, too, are not cures. On average, patients live for about seven years following diagnosis, he said.
In the U.S., women are nearly twice as likely as men to develop AD. Women live longer than men on average, contributing to the increased risk. Women also comprise about two-thirds of dementia caregivers.
“Caregiving for individuals with Alzheimer’s becomes increasingly demanding as the disease progresses, often requiring nearly 24-hour care in the moderate-to-late stages,” Franklin said. “Insurance typically does not cover caregiving costs, placing a financial burden on families. Community support services, such as those provided by the Alzheimer’s Association, can be invaluable.”
A recommendation Franklin offers to caregivers is to maintain a structured routine for individuals with AD since consistent daily activities can help stabilize their sleep-wake cycles and improve overall well-being.
“In addition to managing daily living activities — such as dressing, meal preparation, and feeding — caregivers must also address behavioral changes in patients,” he said. “Having set times for waking up, meals, walks, and social activities can provide stability and promote engagement.”
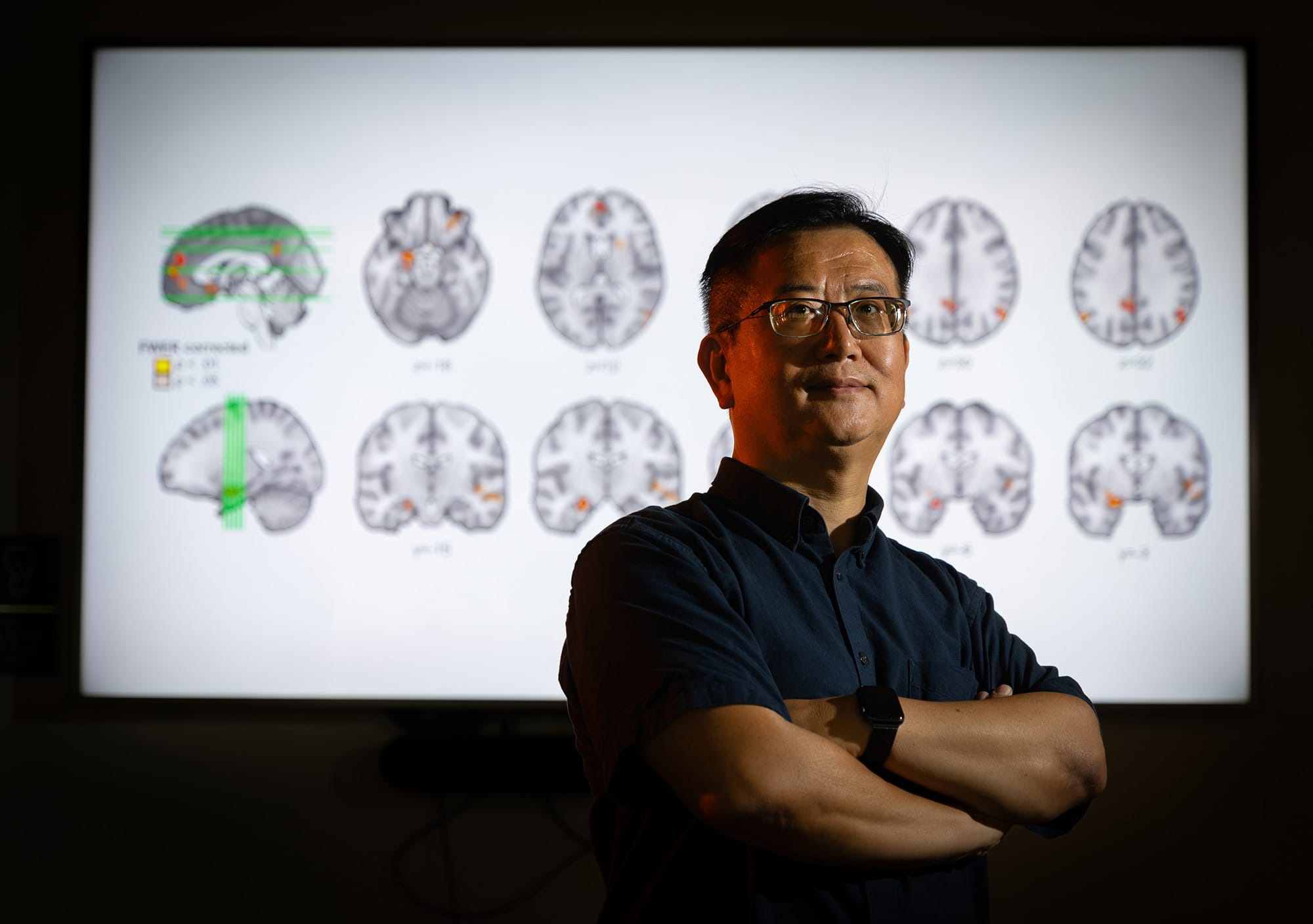
The greatest risk factors for Alzheimer’s dementia are older age, genetics, and having a family history of the disease. Weiwei Zhang, a professor of psychology, combines functional MRI and transcranial electric stimulation — a noninvasive brain stimulation method — to explore how cognitive and motor efforts interact in aging populations. His previous research focused on how memory function and mental health decline with age.
“Mild cognitive impairment is a precursor to Alzheimer’s disease,” he said. “We have extensive data supporting this. Our approach uses cognitive decline as a biomarker to predict AD risk, rather than waiting for mild cognitive impairment to progress to full-blown AD.”
The next step for Zhang is to translate his basic science findings into clinical interventions to slow the progression of dementia. His work with functional MRI and noninvasive brain stimulation aims to connect hippocampal function with memory quality, he said.
Two of several brain changes associated with AD are accumulation of the protein fragment beta-amyloid into clumps (called amyloid plaques) outside neurons and the accumulation of an abnormal form of the protein tau (called tau tangles) inside neurons. But a study by Ryan Julian, a professor of chemistry in the College of Natural and Agricultural Sciences, suggests the root issue may be the cells’ diminishing ability to clear waste, leading to its unhealthy buildup in the brain.
“While traditional research has focused on protein aggregation — initially observed in Alzheimer’s patients — this approach has struggled to clarify the disease’s causes or identify effective treatments,” said Julian, who specializes in analytical science. “About 25% of individuals with plaques show no dementia symptoms, which makes one question their sole role in the disease.”

Julian investigated tau protein’s different forms, or isomers, to uncover more information about the disease mechanism. He discovered that a unique form of tau, differing in its three-dimensional orientation, was present in individuals with dementia and brain plaques or tangles — an indicator of cells’ slowing ability to clean themselves. This finding suggests that examining tau’s isomer forms could help identify those at risk for AD.
“Isomerization is absent in individuals with high protein aggregation but no cognitive issues, indicating a more nuanced connection with brain function,” Julian said. “Additionally, we have found that isomerization varies depending on the nature of genetic mutations associated with early-onset Alzheimer’s. We believe our marker offers new insights beyond conventional analyses and could pave the way for effective therapies and treatments that can make a meaningful difference for those affected by the disease.”
In Alzheimer’s, a hallmark of disease progression is significant cerebral atrophy — decreased brain volume — resulting from neuronal damage, degeneration, and ultimately neuronal loss. While some degree of brain atrophy is common with aging in people who are cognitively healthy, atrophy is accelerated in people with AD and related dementia. Traumatic brain injury, or TBI, is caused by a contusion to the head, and is associated with an increased risk of AD. Moreover, this type of injury, combined with inherited genetic AD risk factors, can accelerate the development of AD and related dementia.
“There’s some literature that suggests that TBI can evolve in some cases to Alzheimer’s or accelerate Alzheimer’s-like symptoms,” said Andre Obenaus, a professor of biomedical sciences, who is co-principal investigator of a three-year, $3.5 million grant from the National Institute of Neurological Disorders and Stroke (NINDS) to examine how and when TBI leads to AD and related dementia.
Using rodents subjected to TBI, Obenaus, in collaboration with his co-principal investigator at the Indiana University School of Medicine, will study three different time periods in the 24-month lifespan of a mouse: the juvenile age, midlife, and late life. The researchers will use cognitive behavioral outcomes, medical neuroimaging such as MRI, immunopathology changes, and tissue biomarkers to assess disease progression.
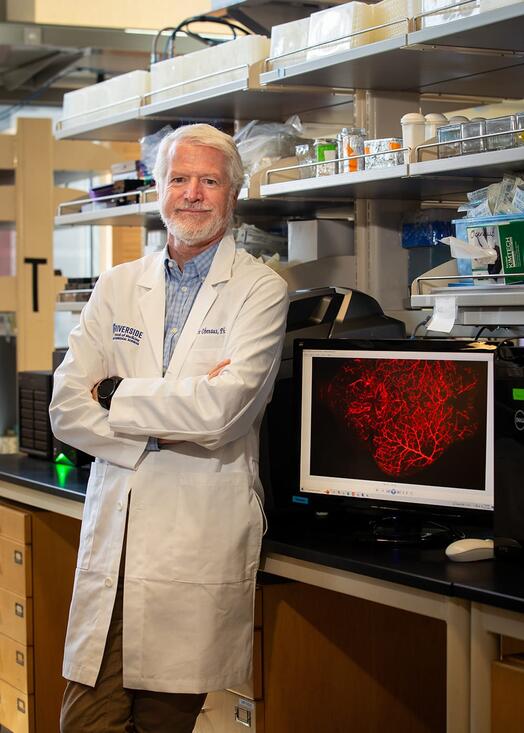
“This system will allow our teams to investigate the interactions of how genetics, aging, and TBI influence AD and related dementia in a well-characterized model system, thus permitting a clearer understanding of how each of these factors contributes to disease progression,” said Obenaus, who is also the principal investigator of a five-year, $3.2 million grant from NINDS to examine blood-borne protein biomarkers of cerebrovascular pathologies in AD and related dementias.
TBI is of interest also to Viji Santhakumar, whose research focuses on understanding memory formation mechanisms and how these can become disrupted in neurological conditions such as epilepsy and TBI — foundational knowledge that can help explain how memory corruption might contribute to the cognitive impairments observed in Alzheimer’s.
“Epilepsy and traumatic brain injury are both highly comorbid with Alzheimer’s disease, and there is considerable overlap in the cellular pathology of these conditions,” said Santhakumar, a professor of molecular, cell, and systems biology. “For example, the tau pathology seen in Alzheimer’s is like that observed in the brain following TBI. Alzheimer’s disease and epilepsy can sometimes be misdiagnosed. Some patients initially diagnosed with Alzheimer’s have been found to experience microseizures in certain brain regions, which can lead to cognitive deficits that mimic Alzheimer’s symptoms.”
Santhakumar is developing collaborations with research institutions to investigate how brain injury may accelerate or exacerbate Alzheimer’s pathology. She is collaborating also with UCR biomedical scientist Devin Binder on a five-year grant of more than $3 million from NINDS to focus on post-traumatic epilepsy. The team will study cellular, molecular, and electrophysiological changes in the brain underlying post-traumatic epilepsy to identify new targets for treatment.
“Many patients experience minor concussions or brain injuries early in life, which may trigger neurocognitive deficits later on,” Santhakumar said. “By studying these processes, we hope to identify potential early treatment options.”

Another researcher, Xiaoping Hu, focuses primarily on developing MRI biomarkers for early detection of Parkinson’s disease, a neurological condition with distinct motor symptoms that is accompanied by uncontrolled movements like shaking and stiffness. Around a third of people with Parkinson’s disease eventually develop AD, according to the Alzheimer’s Society.
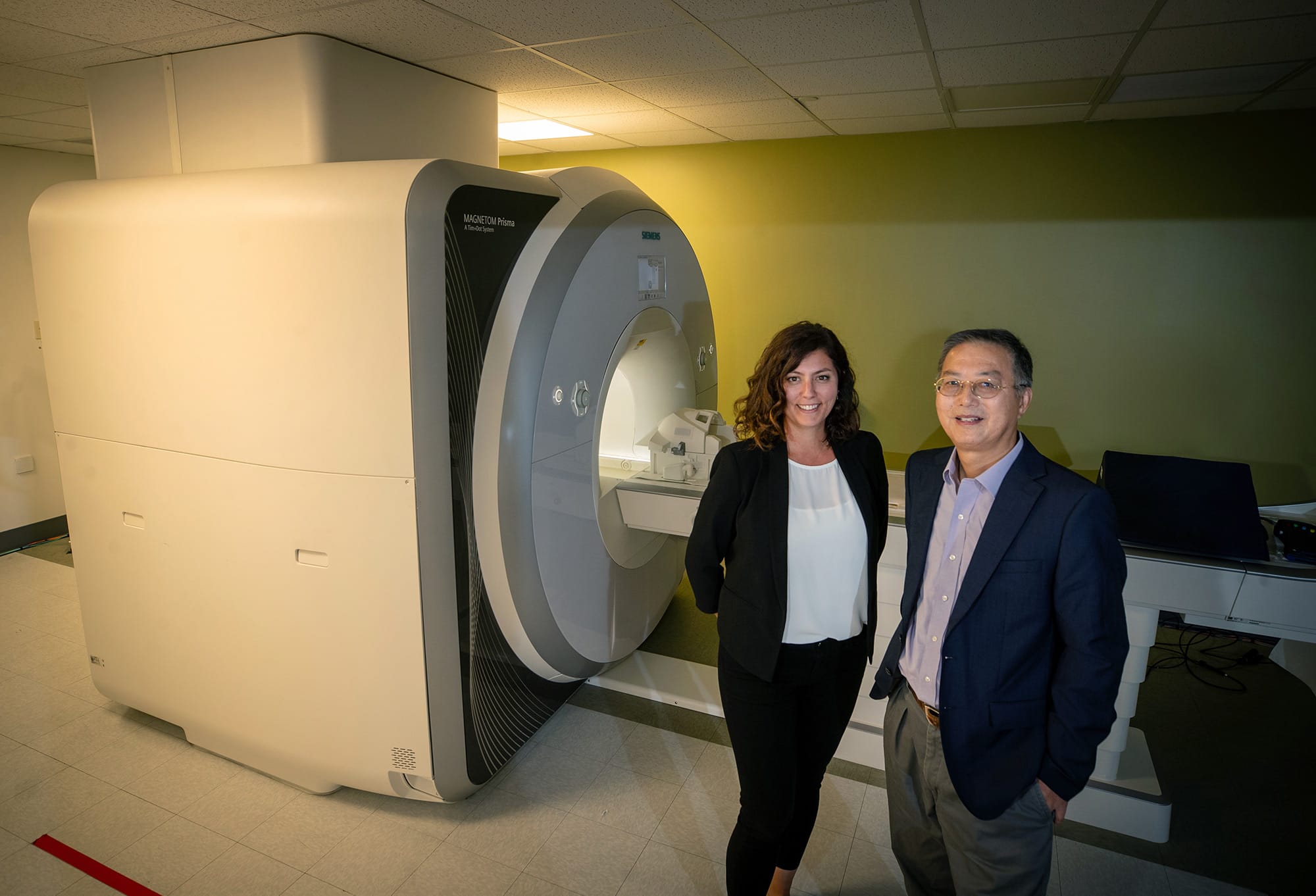
“Our current collaboration with Washington University involves a longitudinal study of individuals with sleep disorders, who have a higher risk — over 20% — of developing Parkinson’s disease,” said Hu, a distinguished professor of bioengineering in the Marlan and Rosemary Bourns College of Engineering and director of the UCR Center for Advanced Neuroimaging (CAN). “This study tracks participants for at least five years, and we’re leveraging a national consortium’s patient registry, which includes clinical measures, blood biomarkers, and sleep studies.”
Hu is applying imaging techniques at CAN, which is equipped with an MRI scanner for brain studies, to also study AD with particular focus on the locus coeruleus, a small, difficult-to-image nucleus in the brainstem that affects sleep, cognition, arousal, and stress regulation.
“Early signs of Alzheimer’s may manifest in the locus coeruleus, so we are investigating its role in normal aging and its potential as an early indicator of dementia,” he said.
With Bennett, Hu is also exploring the relationship between inflammation and dementia, including how it might influence Alzheimer’s progression. For Parkinson’s disease, symptoms such as movement problems, freezing of gait, and other early indicators, such as issues with smell, sleep disorders, and constipation, can precede the disease by several years, typically emerging in people in their 50s or 60s.
“In people with Parkinson’s disease, we have observed degeneration and increased iron levels in specific brain regions, like the locus coeruleus and substantia nigra, which can be visualized with MRI,” Hu said. “These features are hallmarks of Parkinson’s disease but are often detectable only in later stages.”
Hu stressed that, currently, there is no way to reverse neurodegenerative diseases like Parkinson’s or Alzheimer’s once they have progressed, and treatments are only able to manage symptoms.
“Therefore, early diagnosis is crucial, particularly for AD,” he said. “It might enable interventions to slow or halt disease progression.”