By integrating multiple laboratory functions on a chip, microfluidic devices allow lab tests to be performed in a doctor’s office, or in settings with limited health care services. A newly developed silicone-based membrane makes it possible to create micron-scale temperature maps that could help scientists understand how to keep sensitive cells and fragile DNA at optimal temperatures in microfluidic devices. The membrane was developed by an international team of researchers from Universidad Nacional Autónoma de México and the University of California, Riverside.
“Temperature is important for most biological applications and can be critical for achieving accurate biomedical test results,” said Juan Hernández-Cordero, of the Universidad Nacional Autónoma de México. “The membranes we created can be placed on the microchannels in a device so that a technique known as laser-induced fluorescence thermometry can be used to create a detailed temperature map.”
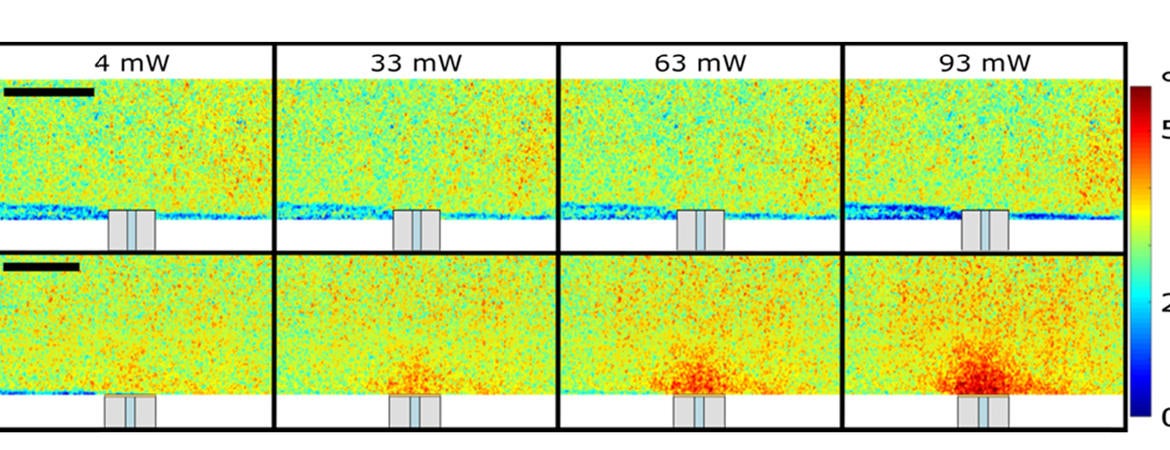
In The Optical Society journal Optical Materials Express, the researchers report their new composite polymer membranes, which are fabricated by simple mixing, and show they can detect temperature changes as small as 1 degree Celsius with a spatial resolution of 2.7 microns per pixel without any damage to the sample. This resolution was high enough to observe heating by light from the tip of an optical fiber.
“We previously developed a simple way of mixing nanostructured materials into polymers,” Hernández-Cordero said. “By following this same procedure we were able to use off-the-shelf materials to make temperature sensitive membranes of any thickness that can be easily replicated in any laboratory.”
During a sabbatical spent with Guillermo Aguilar’s mechanical engineering lab in the Marlan and Rosemary Bourns College of Engineering at UC Riverside, Hernández-Cordero familiarized himself with projects Aguilar’s group had been working on involving optical sensing and laser therapeutic techniques. Some of these techniques are aimed at measuring temperature non-intrusively in liquids and tissue, and others at developing photothermal therapies for treating brain pathologies — in line with the Window to the Brain project that both Hernández-Cordero and Aguilar work on.
“We were developing fiber-optic devices for photothermal therapy, which uses light to generate heat for treating tumors,” Hernández-Cordero said. “We realized that we didn't have a reliable way of measuring the temperature produced by a fiber-optic microheater, which is roughly the size of human hair in thickness.”
“Through our interactions, exchange of ideas, and preliminary experimentation in my lab, the idea of using a similar procedure that uses the new temperature-sensitive membranes described in this paper came to fruition,” Aguilar said.
They examined laser-induced fluorescence thermometry, which measures temperature by using a temperature-sensitive fluorescent dye, rhodamine B. Although it can provide measurements at small scales, the rhodamine must be dissolved, requiring the measurements to be performed in liquid solvents such as water or ethanol. For the fiber-optic microheaters, taking measurements in a liquid would cause problematic bubbles to form due to the high heat generated.
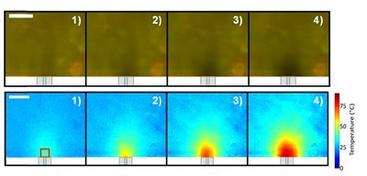
The researchers developed the new temperature-sensitive membranes by simply mixing a type of silicone known as polydimethylsiloxane with rhodamine B. The membranes could be used with laser-induced fluorescence thermometry but without the requirement for taking measurements in liquid solvent. After shining laser light on the membrane, the varying brightness of the fluorescence from the membrane can be imaged and then converted into a map of temperatures across the membrane.
“For photothermal therapy, there are certain temperature ranges that trigger cellular events that are important for therapy to work,” Hernández-Cordero said. “So, in addition to measuring the temperature in the device, the membranes could make it possible to measure the temperature in the tissue samples with high accuracy.”
To test the membranes, the researchers used a hot plate with a precise temperature control system to see how the hot plate temperatures compared with those obtained with the membranes. After this test was successful, they used the membranes to create temperature maps of the fiber-optic microheaters with a heated area of 750 microns by 650 microns.
“Our joint efforts will now focus on developing a thinner membrane to read fast-changing temperature variations with accuracy,” Aguilar said.
“Although for most small-scale applications, fast response times aren’t necessary, a thinner membrane will make it possible to read more dynamic temperature changes,” Hernández-Cordero said. “We want to find out the minimum thickness of the membrane that we can have and still achieve an accurate reading.”
Paper: F. González-Martínez, O. González-Cortez, R. Pimentel-Domínguez, J. Hernández-Cordero, G. Aguilar. “Composite polymer membranes for laser-induced fluorescence thermometry,” Opt. Mater. Express 8, 10, 3072--3081(2018). DOI: https://doi.org/10.1364/OME.8.003072.