Findings by a UC Riverside engineer may lead to advances in pulmonary diagnostics, surgical planning, and artificial ventilation.
Lung disease is the leading cause of death worldwide, but science knows far less about respiratory mechanics than it does about cardiovascular mechanics. Diagnosis between pulmonary diseases is challenging. With a better understanding of lung and airway behavior during health and illness, doctors could make quicker diagnoses and better predict an individual’s risk of serious disease.
Air, which behaves like a fluid, changes the shape of lung tissue during breathing. But scientists lack a fundamental understanding of how breathing pressures cause expansion of the lung tissue and the interaction between air forces and tissue. This blind spot impedes advancements in pulmonary medicine.
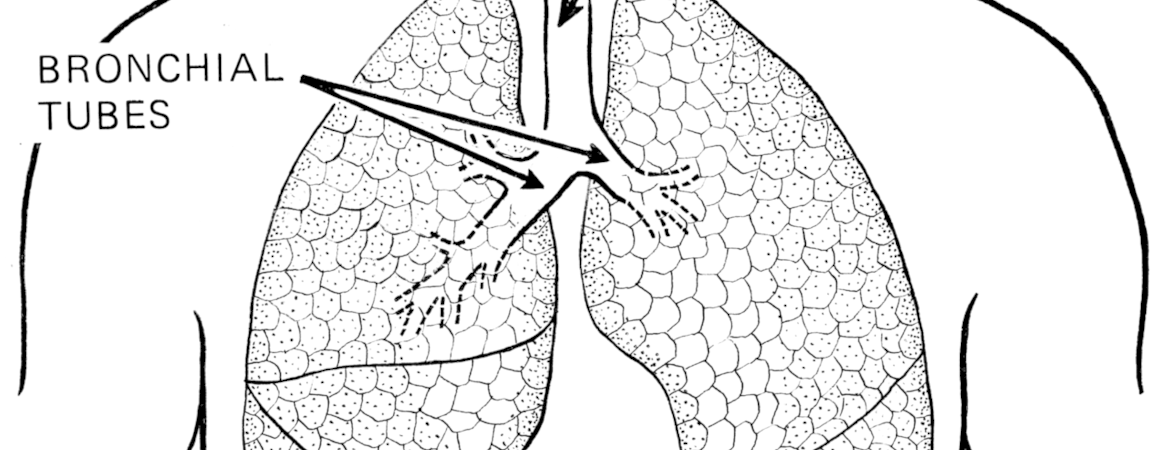
“The mechanical properties of lung and airway tissues are a missing link between lung stresses and strains,” said Mona Eskandari, an assistant professor of mechanical engineering at UC Riverside’s Marlan and Rosemary Bourns College of Engineering, and principal investigator of the bMECH lab, which employs experimental and computational approaches. “If scientists know how breathing deforms the airways and causes forces to be distributed in the bronchial tree, we can create physiological lung models representative of healthy and diseased pulmonary behavior. This would provide physicians with technology to positively impact patients’ lives.”
Eskandari, along with Alberto Arvayo and Marc Levenston at Stanford University, recently published potentially groundbreaking research on airways.
The researchers subjected pig airways to a variety of deformations and measured the resulting forces. They found that the stiffness of the tissue depends not only on the direction, yielding more easily around the edges, but also on the region: smaller air passages are stiffer, contradicting long-standing assumptions.
The study suggested that given the same amount of stretching, greater force could pass through branches farther down the respiratory tract — in airways smallest and farthest away from the trachea, the major tube that air travels down to reach the lungs.
In addition to providing airway tissue measures for use in computer simulations of remodeling and obstruction in diseased airways, the results have possible implications for lung injury caused by ventilators. The findings might help discover ways the lung responds to over-ventilation, leading doctors to reconsider how they artificially ventilate patients.
“This long-term vision relies on investigating the material response of this understudied organ and the experiments we have conducted in this work aims to do just that,” Eskandari said. “The next step is to investigate if human tissue behaves similarly and what happens to the airways when disease causes chronic remodeling and adaptation.”
The paper, “Mechanical Properties of the Airway Tree: Heterogeneous and Anisotropic Pseudoelastic and Viscoelastic Tissue Responses,” was published in the September issue of the Journal of Applied Physiology.




