California residents 65 and older now qualify for COVID-19 vaccinations. Questions about the mRNA Covid-19 vaccines still remain. Vaccine expert Dr. David Lo, a distinguished professor of biomedical sciences and senior associate dean for research in the School of Medicine at the University of California, Riverside, answers several questions in this Q&A:
Besides different storage temperatures for the Pfizer-BioNTech and Moderna vaccines, how do the two vaccines differ from each other in how they work to prevent symptomatic COVID-19?
The Pfizer and Moderna vaccines operate on basically the same basic principle, using a synthetic RNA that codes for a version of the virus spike protein, and injecting it to get your own cells to produce the protein, then get your immune system to initiate an immune response to it. The differences have to do with the way the material is “formulated” which means how the ingredients are all mixed together and packaged. RNA is generally an unstable chemical, so this formulation aspect is important, and both vaccines require very cold storage conditions, with the Pfizer vaccine requiring even more extreme cold to keep it safe. Once thawed, both vaccines have a short shelf life.
Why do we need two doses of either of these vaccines?
We rely on the immune system to provide protection by producing antibodies as well as developing what is called immune memory that keeps producing those antibodies for a long time. That means that a faster and stronger immune response is generated when a booster shot is given to provide a second exposure to the same antigen, and the immunity is also much longer lasting after a booster. Most of our best vaccines require at least two doses, such as the Hepatitis B vaccine, Shingles vaccine, tetanus and so on. Reminder – get your tetanus booster every 10 years!
Why do the two doses need to be taken weeks apart?
The initial priming dose triggers the initial immune response, but our bodies’ immune system starts off as naïve, with no prior experience with the virus antigens. The second dose can be very important in giving the immune system a second kick to essentially build a sufficiently strong defense structure against the potential exposure to live virus. That means having the immune system start producing enough antibodies that can neutralize any virus that comes along.
Is the second, top-up dose the same as the first, priming dose in composition, strength, and interaction with the immune system?
For simplicity in formulation or dosing, the second dose does not need to be any different from the priming dose. The immune system will ramp up in response to the booster in any case.
How effective is the first dose without the second?
The second dose can be really important in making sure you have an adequate immune response. Maybe one possible analogy would be to how we learn some complex material in a class. A few lucky people might learn the information straight off with no need for review or reminder booster shots, but most people need to review and repeat to get the information solidly in your head.
Will delaying the second dose make the vaccine less effective overall?
The timing of the second dose is a guess that the immune response to the first priming dose needs to be reminded in a relatively short period so that the system doesn’t fully calm down and forget what it saw. So, in principle, the booster should not be delayed too long.
Does the timing of the second dose affect the overall efficacy of the vaccine?
There is a bit of an art to this, and vaccine developers are limited in not having the time or money to test every single last possible variation. As a result, the different vaccines have to be tested according to a best guess as to dose, and timing of the second dose. The FDA, in order to protect patients, has to ensure that vaccine approval is based on the results from testing of strictly applied vaccination protocols, or it cannot fully evaluate and insure whether the vaccine actually protects.
Are the available COVID-19 vaccines effective against new strains of the coronavirus?
Infectious diseases are always changing and mutating. In some cases, for example, bacteria can mutate to be resistant to antibiotics. In the case of viruses, some viruses, such as influenza, change very rapidly, so each year we need a new flu vaccine. So far, the COVID-19 virus does not appear to be changing very rapidly and the vaccines being developed now seem to be quite adequate.
Can you still pass on the coronavirus to others after receiving the vaccine?
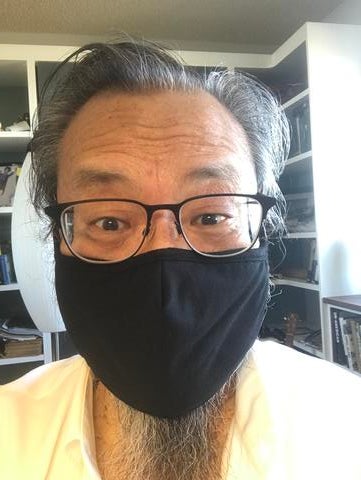
We’re still learning about the virus and immunity. Since the immunity from vaccination can take time to fully develop, it has happened that people got infected even after they received the first dose of vaccine, in some cases because they were exposed before immunity had a chance to develop. Some people have still gotten infected after vaccination but they were protected from having more severe or lethal disease. Also, it is known that the response to vaccination is not 100% for any vaccine (including flu, hepatitis, etc.); we’re relatively lucky that the present COVID vaccines are as effective as they are. So: wear your mask even after you get the vaccine!
Why are masks and physical distancing still being recommended for people who have received the vaccine?
There are two parts to this question. First, we are still learning whether the vaccination will prevent spread among infected patients. We do know that vaccination will reduce symptoms and disease severity in vaccinated patients who actually get infected, but we’re not yet sure whether it prevents spread. The second part of this is that we need the community at large to get used to the idea that masks make a big difference in health, and this has benefits for other infectious diseases as well. This is not our first, nor will it be our last pandemic, and protecting ourselves and others as a community should not be a political issue.