Bacteria, fungi, and viruses can enter our gut through the food we eat. Fortunately, the epithelial cells that line our intestines serve as a robust barrier to prevent these microorganisms from invading the rest of our bodies.
A research team led by a biomedical scientist at the University of California, Riverside, has found that simulated microgravity, such as that encountered in spaceflight, disrupts the functioning of the epithelial barrier even after removal from the microgravity environment.
“Our findings have implications for our understanding of the effects of space travel on intestinal function of astronauts in space, as well as their capability to withstand the effects of agents that compromise intestinal epithelial barrier function following their return to Earth,” said Declan McCole, a professor of biomedical sciences at the UC Riverside School of Medicine, who led the study published today in Scientific Reports.
The microgravity environment encountered in space has profound effects on human physiology, leading to clinical symptoms and illnesses including gastroenteritis; previous studies have shown microgravity weakens the human immune system. Microgravity has also been shown to increase the intestinal disease-causing ability of food-borne bacteria such as salmonella.
“Our study shows for the first time that a microgravity environment makes epithelial cells less able to resist the effects of an agent that weakens the barrier properties of these cells,” McCole said. “Importantly, we observed that this defect was retained up to 14 days after removal from the microgravity environment.”
The permeability-inducing agent McCole’s team chose to investigate was acetaldehyde, an alcohol metabolite. McCole explained alcohol compromises barrier function and increases gastrointestinal permeability in normal subjects and in patients with alcoholic liver disease.
The barrier function of the intestinal epithelium, he added, is critical for maintaining a healthy intestine; when disrupted, it can lead to increased permeability or leakiness. This, in turn, can greatly increase the risk of infections and chronic inflammatory conditions such as inflammatory bowel disease, celiac disease, Type 1 diabetes, and liver disease.
McCole’s team used a rotating wall vessel — a bioreactor that maintains cells in a controlled rotation environment that simulates near weightlessness — to examine the impact of simulated microgravity on cultured intestinal epithelial cells.
Following culture for 18 days in the vessel, the team discovered intestinal epithelial cells showed delayed formation of “tight junctions,” which are junctions that connect individual epithelial cells and are necessary for maintaining impermeability. The rotating wall vessel also produces an altered pattern of tight junction assembly that is retained up to 14 days after the intestinal epithelial cells were removed from the vessel.
“Our study is the first to investigate if functional changes to epithelial cell barrier properties are sustained over time following removal from a simulated microgravity environment,” McCole said. “Our work can inform long-term space travel and colonization where exposure to a food-borne pathogen may result in a more severe pathology than on Earth.”
McCole was joined in the study by Rocio Alvarez, Cheryl A. Stork, and Anica Sayoc-Becerra of UC Riverside; and Ronald R. Marchelletta and G. Kim Prisk of UC San Diego.
The research was funded by grants from the National Institutes of Health and NASA.
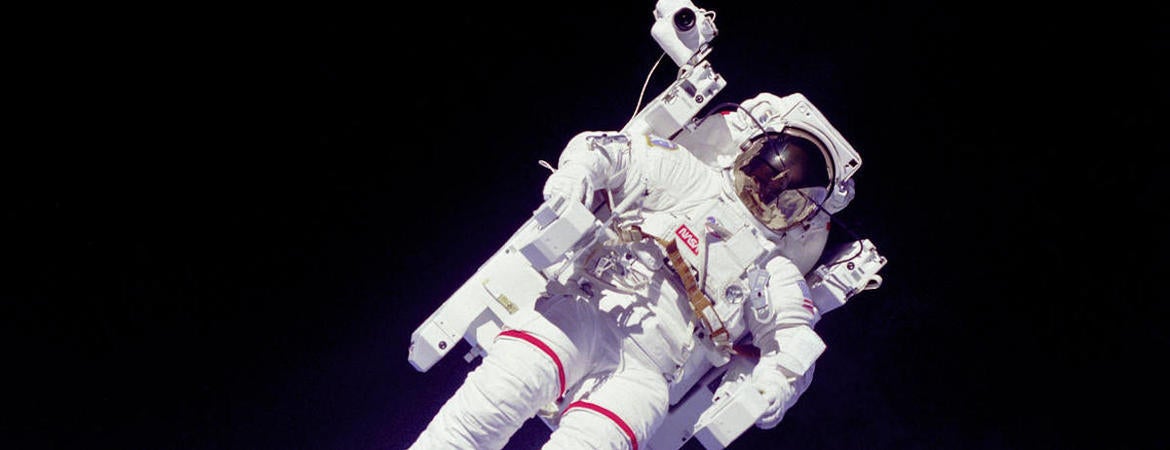
Header image credit: NASA.




