Scientists have long thought of the fluid-filled sac around our lungs merely as a cushion from external damage. Turns out, it also houses potent virus-eating cells that rush into the lungs during flu infections.
Not to be confused with phages, which are viruses that infect bacteria, these cells are macrophages, immune cells produced in the body.
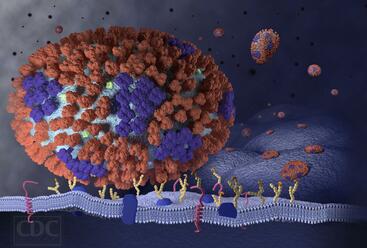
“The name macrophage means ‘big eater.’ They gobble up bacteria, viruses, cancer cells, and dying cells. Really, anything that looks foreign, they take it up and destroy it,” said UC Riverside virologist Juliet Morrison, who led the discovery team. “We were surprised to find them in the lungs because nobody has seen this before, that these cells go into the lung when there’s an infection.”
A paper published in the Proceedings of the National Academy of Sciences details how during an influenza infection, macrophages leave the exterior cavity and cross into the lungs where they decrease inflammation and reduce levels of disease.
“This study shows it’s not just what happens in the lung that matters, but also what’s outside of the lung. Cell types not normally connected to the lung can have outsized impacts on lung disease and health,” Morrison said.
There are three main cavities in the body: one around the heart, the abdominal cavity, and the pleural cavity surrounding the lungs. “Because it contains fluid, it prevents the lungs from collapsing. However, people have not thought much about the pleural cavity being a whole organ within itself. This research may change that perception,” Morrison said.
Initially, the researchers set out to understand the more general question of what types of cells are present in the lungs during flu infections. They took existing data on lung-related genes from studies of mice that either died from the flu or survived. They then mined the data using an algorithm to predict cell types that change in the lungs during infections.
“We took big data and broke it down to assign which potential immune cells are in the lung tissues. That’s where I got a hint that maybe we had a previously unknown external source of cells in the lung,” Morrison said.
Next, using a laser-based technique, the team tracked macrophages going into the lungs of mice, and observed what happened if they took these cells out of the equation. “When you take them out of the mouse you see more disease and more lung inflammation,” Morrison said.
Morrison says she hopes this study will encourage other scientists to reevaluate data sets from older studies. “Our approach was to take information already out there and put it to new use, and we were able to see something new,” she said.
Moving forward, the research team is hoping to determine which proteins “tell” the macrophages to move into the lungs. Once the protein signals have been identified, it may be possible to create drugs that boost either the number of macrophages, or their activity.
The strategy of boosting human defenses to infection, rather than developing another antiviral, could offer people a flu treatment that would be more effective for much longer. Morrison became interested in host therapeutics because antibiotic and antiviral resistance to drugs is a growing problem.
This problem occurs when germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them. Misuse and overuse of the drugs is accelerating the problem. According to the Centers for Disease Control and Prevention, more than 2.8 million drug-resistant infections occur each year in the U.S., and more than 35,000 people die as a result.
“If we can boost what resolves infection in us, we probably have a better shot. We’re less likely to have resistance. The immune system is so complicated, but it’s our best bet in the long run to work with what we have rather than chase viruses that continue to escape our therapeutics,” Morrison said.
(Cover image: magicmine/iStock/Getty)